Syndromes
Summary.
This review was presented by Pure Dentistry Dentists in Brisbane.
Cleidocranial Dysplasia Syndrome:
- autosomal dominant skeletal dysplasia, 1 per million
- mutation in RUNX2
- delayed closure of the cranial sutures & hypoplastic or aplastic clavicles
- dental abnormalities
o supernumerary
o retained primary dentition & failure of eruption of permanent teeth
o crowding
Turner Syndrome:
common chromosomal abnormalities effecting women with complete or partially missing X chromosome.
1 in in 2000 live births.
- Short stature- lower leg and arm can be shorter than the upper leg and arm
- Infertility due to ovarian failure, Lymphoedema, Webb neck, Cardiac and renal abnormalities, Skeletal defects, micrognathia, cubitus Valgus, short neck, high-arched palate, short metacarpals, genu valgum, scoliosis, madelung deformity, Usually normal intelligence but may have some problems with social and psychomotor skills
- Tooth abnormalities: early eruption of the secondary teeth, simple crown morphology, thinner enamel, less dentine, short roots
Noonan Syndrome:
- autosomal dominant, pulmonary valve stenosis, small stature, hypertelorism, mild intellectual disability, ptosis, undescended testes, and skeletal malformations.
- 1 in 1000–2500
- Mutations in genes that are part of the RAS/RAF/MEK/ERK signal transduction pathway
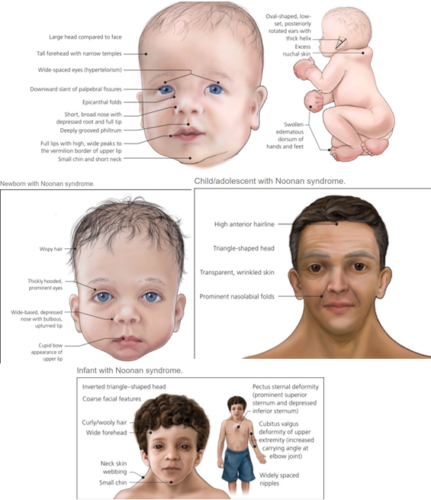
- Facial features include: Triangular-shaped face, Hypertelorism, Down-slanting palpebral fissures, Ptosis, Strabismus, Amblyopia, Refractive errors, Low-set ears with thickened helices, High nasal bridge, Short, webbed neck.
- oral manifestations included micrognathia, high arch palate, malocclusion, impacted teeth, Early exfoliation of primary, supernumerary teeth, taurodontism,
Klinefelter Syndrome:
- set of physical, language, and social development symptoms in males who have an extra X chromosome
- 1:650 newborn males
- Narrow shoulders, Broad hips, Absence or sparse facial, axillary, pubic and body hair, Gynecomastia & Feminine distribution of adipose tissue, Small testes and penis, Androgen deficiency, Reduced intelligence
- Taurodontism
- Differebtial Diagnosis: Fragile X-syndrome, Kallman syndrome, Marfan syndrome
Ectrodactyly- Ectodermal Dysplasia Clefting Syndrome:
- lobster-claw anomaly hands/feet, obstruction of nasolacrimal duct & cleft lip& palate.
- 5/100 million
- autosomal dominant, t mutation in the TP63 or TP73L genes
- ectrodactyly, ectodermal dysplasia, cleft palate and/or cleft lip
- Hypodontia and anodontia , Reduced growth rate alveolar processes, Microdontia , Enamel hypoplasia , Misshapen teeth , Taurodontism , Xerostomia
Cleidocranial Dysplasia Syndrome:
Description:
Cleidocranial dysplasia (CCD) is an autosomal dominant skeletal dysplasia characterised by patency of the anterior fontanelle, inverted pear-shaped calvaria, hypertelorism, general midface retrusion and mandible prognathism, associated with an excessive mobility of the shoulders, short stature and teeth abnormalities such as supernumerary teeth and failure of eruption (Farrow et al. 2018). The name dysostose cleido-cranienne hereditaire (hereditary cleidocranial dysostoses) was used by Pierre Marie and Paul Sainton in 1898.
Other names:
- Cleidocranial Dysostosis
- Marie-Sainton Syndrome
- Mutational dysostosis
Prevalence:
Cleidocranial Dysplasia (CCD) is a rare congenital disorder with prevalence of 0.5/100,000 live births (Brueton et al.1992). A more recent update in 2017 reported the prevalence to be 1 per million individuals worldwide (Machol et al. 2006 [updated 2017]).
Genetics:
CCD is caused by mutation in the RUNX2 gene on the short arm of chromosome 6 (6p21). Inheritance is autosomal dominant. It may be inherited from an affected parent or occur due to a new mutation in the RUNX2 gene. This gene provides instructions for making a protein that is involved in the development and maintenance of teeth, bones and cartilage. Due to mutation in RUNX2 (CBFA1) the protein produced from one copy of the RUNX2 will be eliminated or reduced. It is believed that the RUNX2 protein acts as a “master switch,” regulating a number of other genes involved in the development of osteoblasts and teeth. In rare cases, individuals with a deletion of genetic material that includes RUNX2 and other nearby genes may experience additional features, such as developmental delay, resulting from the loss of these genes. In about 30 percent of individuals with cleidocranial dysplasia, no mutation in the RUNX2 gene has been found. The cause of the condition in these individuals is unknown (Bruderer et al. 2014, Mundlos et al. 1997).
Clinical characteristics: (K. Machol et al. 2017)
Clinical presentation of CCD can range from the classical triad of delayed closure of the cranial sutures, hypoplastic or aplastic clavicles and dental abnormalities to mild CCD to isolated dental anomalies without the skeletal features (Golan et al. 2003).
- Abnormally large, wide-open fontanelles at birth that may remain open throughout life.
- Frontal and parietal bossing and mid-face retrusion
Narrow, sloping shoulders that can be opposed at the midline due to clavicular hypoplasia or aplasia. As the photo below shows shoulders in an individual with clavicular hypoplasia may be brought to the midline

- Abnormal dentition including
o delayed eruption of secondary dentition
o retained primary dentition
o supernumerary teeth
o dental crowding
o malocclusion
- Hand abnormalities including
o Brachydactyly (shortness of the fingers and toes)
o tapering fingers
o short &broad thumbs
- Short stature (typically moderate)
Normal intellect in individuals with classic CCD spectrum disorder
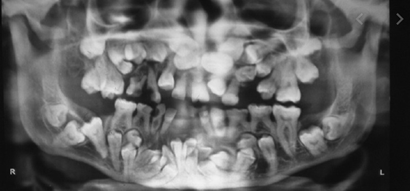
Radiographic findings
- Cranium
o Wide-open sutures, patent fontanelles, presence of wormian bones (small sutural bones)
o Delayed ossification of the skull
o Poor or absent pneumatization (air spaces) of the paranasal, frontal, and mastoid sinuses
o Impacted, crowded teeth and supernumerary teeth
- Thorax
o Cone-shaped thorax with narrow upper thoracic diameter
o bilateral (but not necessarily symmetric) clavicular abnormalities ranging from complete absence to hypoplastic or discontinuous clavicles.

o Hypoplastic scapulae
- Pelvis
o Delayed ossification of the pubic bone with wide pubic symphysis
o Hypoplasia of the iliac wings
o Widening of the sacroiliac joints
o Elongated femoral head with short femoral neck and elongated epiphyses (“chef-hat” appearance)
o Coxa vara
- Hands
o Pseudoepiphyses of the metacarpal and metatarsal bones, which may result in a characteristic lengthening of the second metacarpal.
o Hypoplastic distal phalanges
o Deformed and short middle phalanges of the third, fourth, and fifth digits with cone-shaped epiphyses

- Osteopenia/osteoporosis with evidence of decreased bone mineral density
Height:
Individuals with CCD spectrum disorder are often shorter than their unaffected sibs:
- Males are on average six inches shorter than their unaffected brothers and have an average height of 165 cm (±8 cm).
- Females are on average three inches shorter than their unaffected sisters and have an average height of 156 cm (±10 cm) (Cooper et al. 2001).
Skeletal/orthopedic problems:
Affected individuals are more likely to have other bone-related problems:
- Pes planus (flat feet) in 57%
- Genu valgum (knock-knee deformity) in 28%.
- Scoliosis in 18% (Cooper et al. 2001).
- Osteoporosis, osteopenia (Cooper et al. 2001).
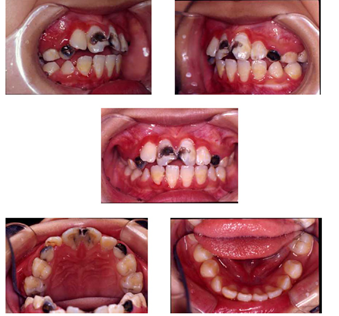
Dental complications
- Up to 94% of persons with CCD will have dental findings including:
o Retained primary teeth.
o Eruption failure of permanent teeth (Golan et al. 2003).
o Presence of second primary molars with the presence of the second permanent molar with the primary dentition (80%) (Cooper et al. 2001).
o Wide spacing in the lower incisor area (Golan et al. 2003).
o Supernumerary tooth germs (70%) (Golan et al. 2004).
o Parallel-sided ascending rami (Bufalino et al. 2012).
o Underbite and cysts in their gums that usually form around supernumerary teeth. (McNamara et al. 1999).
o Teeth abnormalities include enamel and cementum hypoplasia, root dilaceration, and microdontia. Submucous cleft palate as well as complete cleft of hard and soft palates have also been reported (Winter 1943).
ENT complications
- Recurrent sinus infections and other upper-airway complications.
- Conductive hearing loss.
- Recurrent ear infections.
Endocrinology
- low IGF-1(Insulin-like growth factor 1) levels.
- Low vitamin D with no consistent association with osteoporosis (Dincsoy Bir et al. 2017).
- Rarely, low levels of alkaline phosphatase (El-Gharbawy et al. 2010; Morava et al. 2002; Unger et al. 2002).
Development
- Intelligence is typically normal.
- Children younger than age five years may show mild motor delay, particularly in gross motor abilities.
Diagnosis:
- Based on clinical and radiographic findings
- Molecular genetic testing (RUNX2)
- Prenatal diagnosis via ultrasound as early as 14 weeks gestation
Differential Diagnosis:
- Mandibuloacral dysplasia: progressive disorder characterised by short stature, delayed closure of cranial sutures, mandibular hypoplasia, dysplastic clavicles, hypoplastic roots leading to early tooth loss, decreased subcutaneous fat.
- Pycnodysostosis: pathogenic variants in the gene that encodes cathepsin K, a lysosomal protease excreted by the osteoclasts for bone matrix degradation. Charcterised by short stature, osteoporosis, short terminal phalanges and failure of closure of cranial sutures
- Yunnis Varon syndrome: prenatal growth deficiency, wide-open fontanels and sutures, unusual mineralisation of the skull and hypoplastic clavicles. Caused by mutation of FIG4.
- CDAGS syndrome: characterised by craniosynostosis, delayed closure of the fontanels, cranial defects, clavicular hypoplasia, anal and genitourinary malformations, skin eruption.
- Hypophosphatasia: characterized by a generalized defect of mineralization with delayed ossification of multiple skeletal elements. Children with the infantile form may present with very poorly mineralized cranium, widened cranial sutures, short ribs, and narrow thorax. The alkaline phosphatase activity in serum and tissues is very low.
- Crane-Heise syndrome: rare syndrome characterized by poorly mineralised calvarium, facial dysmorphism, vertebral abnormalities and absent clavicles.
Dental considerations:
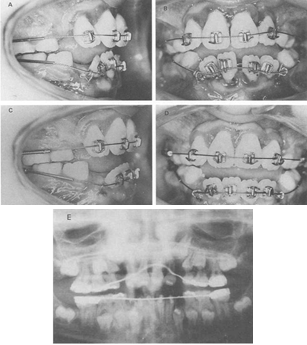
The dental problems that need to be addressed include the retention of deciduous dentition, the presence of supernumerary teeth, and the non-eruption of the permanent dentition.
The goal of treatment is to improve appearance and to provide a functioning masticatory mechanism. The goals may be achieved with prosthetic replacements, with or without prior extractions; by removal of the supernumerary teeth followed by surgical repositioning of the permanent teeth; and by a combination of surgical and orthodontic measures for actively erupting and aligning the impacted permanent teeth. Careful planning of anaesthetic management due to craniofacial and dental abnormalities to secure the airway should be done (K. Machol et al. 2017)
Various treatment strategies have been proposed in terms of timing of extractions and exposures. Becker et al. have reviewed some of these methods in 1997 (Becker et al. 1997).
The four well-known surgical-orthodontic treatments are the Toronto-Melbourne, Belfast-Hamburg, Jerusalem, and Bronx approaches.
The Toronto-Melbourne approach (Hall & Hyland, 1978; Smylski, Woodside, & Harnett, 1974) is based on age. The best period for treatment begins at 5 to 6 years of age. The timing of serial extraction of primary teeth depends on the extent of the root lengths developed in permanent teeth. Supernumerary teeth are also extracted with the alveolar bone covering the impacted teeth. Rationale of this approach is to facilitate the spontaneous eruption of impacted permanent teeth, so there would be no need for orthodontic traction.
The Jerusalem approach needs 2 surgical procedures. In the first phase, the anterior primary teeth and all supernumerary teeth are extracted, followed by the exposure of permanent incisors at 10 to 12 years of age. In the second phase, the posterior primary teeth are extracted, and the impacted permanent canines and premolars are exposed after age of 13. The surgery removes the barrier on the eruption path and promotes the normal eruption pattern of impacted teeth. However, if two-thirds of the roots in permanent teeth have already developed in this approach, further orthodontic traction is usually needed.
The Belfast-Hamburg approach is similar to Jerusalem approach, though the age is not specified. Only one surgery under general anaesthesia is advocated to remove all primary and supernumerary teeth, and to expose the impacted permanent teeth. After healing orthodontic traction is performed.
In the Bronx approach, the first phase is to remove primary teeth as well as supernumerary teeth and expose the impacted teeth. The use of removable partial overdenture is for aesthetic and functional purposes. Orthodontic treatment starts after the spontaneous eruption of permanent teeth for sufficient posterior support, then orthognathic surgery is performed. Finally, implants are placed to restore dentition defects.
Each approach has different indications and outcomes. The skeletal anomalies and complex multiple dentition of CCD add much difficulty and uncertainty to the orthodontic treatment. The treatment method of CCD is still under exploration.
A recent study by Jensen & Kreiborg looked at longitudinal clinical and radiographic data collected by Professor Arne Björk, during the period 1953–1971, and these data were combined with data collected by Jensen & Kreiborg over the years. Based on these data they found (Kreiborg and Jensen 2018):
- The dental lamina for the primary and permanent dentition is normal in CCD.
- The succeeding dental lamina and the lamina for the permanent molars do not completely regress at the expected time.
- At the time when the crown of each successional permanent tooth is completed, remnants of the dental lamina may become re‐activated to form a supernumerary tooth, delayed about 4 yr compared with the first formed permanent tooth, but, in principle, similar to the first formed permanent tooth and localized incisally/occlusally and orally to the first formed permanent tooth.
- The dental lamina for the permanent molars does not regress at the expected time. In these cases, the dental lamina extends distally to form supernumerary molars with the expected time intervals as seen in the sequential formation of the first, second, and third molars.
- Abnormalities of crown and root morphology in the supernumerary teeth can be considered as secondary to the inadequate space conditions in the jaws during their development.
- Abnormalities of root morphology in the first formed permanent teeth can be considered to be secondary to arrested eruption.
- Ectopic location of first formed permanent teeth is caused by migration secondary to arrested eruption and interference with supernumerary teeth in the region.
- Severely delayed or arrested eruption of the first formed permanent teeth (even in regions without supernumerary teeth) is probably caused primarily by diminished bone resorption and diminished resorption of the roots of the primary teeth, and secondarily by the presence of multiple supernumerary teeth in the eruption pathway.
There has been a case report of a 26-year-old man with CCD and odontoma at the anterior maxillary region causing repeated and refractory dental infections. While supernumerary teeth and dental malformations are expected in CCD, the existence of odontomas (ODs) and OD-related infections are less common (Martins et al. 2019).
Turner Syndrome:
Description:
Turner syndrome was first described by Henry Turner in 1938. It is one of the most common chromosomal abnormalities effecting women (Turner 1938). It is a condition with complete or partially missing X chromosome. If the chromosomal anomaly is only present in some cells, it is known as Turner syndrome with mosaicism, which is less sever and has fewer symptoms. More than 95% of adult women with Turner syndrome have a short stature and infertility.
Other names:
- 45,X
- Monosomy X
- TS
- Turner’s syndrome
- Ullrich-Turner syndrome
Prevalence:
1 in in 2000 live births. The condition is much more common in utero, being estimated that 1-2% of all conceptuses are affected, of whom only 1% will survive to term (Donaldson et al. 2006).
Genetics:
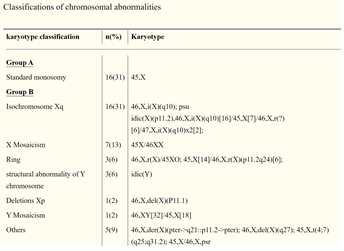
Turner syndrome is caused by the absence of one set of genes from the short arm of one X chromosome. In patients with 45,X karyotype, about two thirds are missing the paternal X chromosome. In addition to monosomy X, a similar clinical picture is found with a 46,XXiq karyotype and in some individuals with mosaic karyotypes. A deletion of the SHOX gene can cause a similar skeletal phenotype known as Leri-Weill dyschondrosteosis.
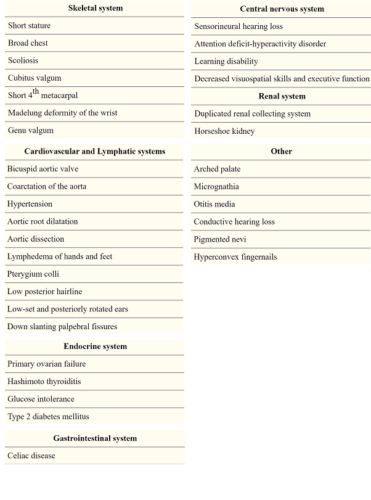
Characteristics (Ogata and Matsuo 1995):
- Short stature- lower leg and arm can be shorter than the upper leg and arm
- Infertility due to ovarian failure
- Lymphoedema
- Webb neck
- Cardiac and renal abnormalities
- Skeletal defects, micrognathia, cubitus Valgus, short neck, high-arched palate, short metacarpals, genu valgum, scoliosis, madelung deformity
- Usually normal intelligence but may have some problems with social and psychomotor skills

Phenotypic features of turner syndrome (Folsom and Fuqua 2015):
Diagnosis:
Prenatal: Turner syndrome may be diagnosed by amniocentesis or chorionic villus sampling during pregnancy. On fetal ultrasonography, Turner syndrome is suggested by the presence of a nuchal cystic hygroma (Alpman et al. 2009), horseshoe kidney, left-sided cardiac anomalies, or nonimmune fetal hydrops, unconjugated estriol and alpha-fetoprotein in maternal serum, abnormal levels of chorionic gonadotropic can be seen in older mothers (Sybert and McCauley 2004).
Natal: Newborns with Turner syndrome usually have increased risk of cardiac (hypoplastic left heart, edema) and kidney (horseshoe shaped) anomalies. Puffy hands and feet, residual effects of cystic hygroma in utero and excess skin around the neck can also be seen in newborns with Turner syndrome (Sybert and McCauley 2004).
Childhood: definite diagnosis is usually by karyotyping. Short posture should also be well investigated.
Other laboratory tests that may be useful in diagnosis of Turner Syndrome include:
- Gonadotropins: Both LH and FSH may be elevated in untreated patients younger than 4 years; they are later suppressed to normal or near-normal levels, only to rise to menopausal levels after age 10 years (Conte et al. 1975).
Thyroid function tests: Because of the high prevalence of in Turner syndrome (Pai et al. 1977) thyroid hormones should be evaluated.
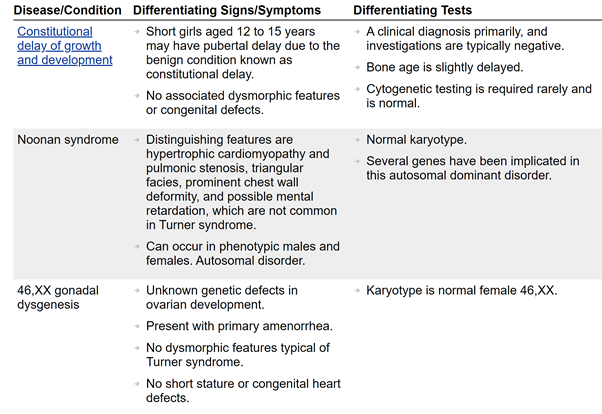
Differential Diagnosis:
Dental Considerations:
Distinct craniofacial features in TS include
- Flattened cranial base angle.
- Marked reduction in posterior cranial base length.
- Retrognathic face (Rongen-Westerlaken et al. 1992).
- Maxilla is generally narrow with a high, arched palate, whereas the mandible tends to be wide and micrognathic (Ogata and Matsuo 1995, Lopez et al. 2002).
- The prevalence of distal molar occlusion, anterior and lateral open bite, and lateral crossbite are significantly increased (Midtbø and Halse 1996).
Abnormalities in tooth development and morphology include
- early eruption of the secondary teeth
- simple crown morphology
- thinner enamel
- less dentine
- short roots (Zilberman et al. 2000).
Girls with TS are also at greater risk for root resorption, which can lead to tooth loss, especially during orthodontic treatment.
It is recommended that all girls with TS see a paediatric dental specialist in Brisbane by the age of 2 years and an orthodontist no later than age seven years.
Because GH treatment can alter craniofacial proportions, all girls with TS treated with GH should receive periodic orthodontic follow-ups (Russell 2001).
Prophylactic antibiotics may need to be used before dental procedures in TS with known cardiac malformations.
Oral manifestations of celiac disease should also be considered in patients with Turner Syndrome (Rashid et al. 2011). These include:
o Enamel defect
o Delayed eruption
o Recurrent aphtus ulcers
o Cheilosis & Atrophic glossitis
o Oral lichen planus
Noonan Syndrome (NS)
Description:
Noonan syndrome is an autosomal dominant, variably expressed, multisystem disorder It was characterised by Jacqueline Noonan, who reported nine patients with pulmonary valve stenosis, small stature, hypertelorism, mild intellectual disability, ptosis, undescended testes, and skeletal malformations (Noonan 1963).
Other known names:
- Male Turner syndrome
- Noonan-Ehmke syndrome
- Turner-like syndrome
- Ullrich-Noonan syndrome
- In 1949, Otto Ullrich reported affected individuals and noted a similarity between their features and those in a strain of mice bred by Bonnevie (webbed neck and lymphedema). The term “Bonnevie-Ullrich syndrome” became popular, particularly in Europe. (Allanson and Roberts 1993).
Prevalence:
- estimated prevalence of 1 in 1000–2500 (Mendez and Opitz 1985)
- mild cases may be as common as one in 100 live births
Genetics:
NS is a common autosomal dominant condition. Mutations in genes that are part of the RAS/RAF/MEK/ERK signal transduction pathway, an important regulator of cell growth. Approximately 50% of patients have gene mutations in PTPN11, with SOS1 and RAF1 mutations identified in another 13% and 5-17% of patients, respectively. Mutations in KRAS, NRAS, BRAF, and MAP2K1 also have been identified, but in smaller numbers of patients.
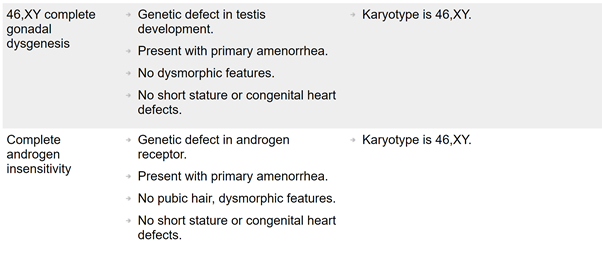
Diagnosis:
Prenatal features: Advanced paternal age has been observed in cohorts with NS (Tartaglia et al. 2004). Common perinatal findings include polyhydramnios, lymphatic dysplasia including increased nuchal translucency and cystic hygroma, relative macrocephaly, and cardiac and renal anomalies (Myers et al. 2014).
Gene mutations identified in individuals with the NS phenotype are involved in the Ras/MAPK (mitogen-activated protein kinase) signal transduction pathway and currently explain about 61% of NS cases.
NS frequently remains a clinical diagnosis (Bhambhani and Muenke 2014).
Characteristics:
It is characterised by a pattern of typical facial dysmorphism and malformations including congenital cardiac defects, short stature, abnormal chest shape, broad or webbed neck, and a variable learning disability. Mildly affected adults may not be diagnosed until the birth of a more obviously affected child. The phenotype is highly variable (Turner 2014).
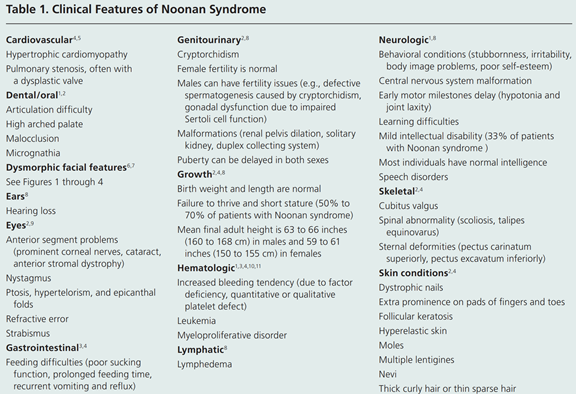
Facial features include:
o Triangular-shaped face
o Hypertelorism
o Down-slanting palpebral fissures
o Ptosis
o Strabismus
o Amblyopia
o Refractive errors
o Low-set ears with thickened helices
o High nasal bridge
o Short, webbed neck
Differential Diagnosis:
Turner syndrome:
found only in females, is differentiated from Noonan syndrome (NS) by demonstration of a sex chromosome abnormality on cytogenetic studies in individuals with Turner syndrome. In Turner syndrome renal anomalies are more common, developmental delay is much less frequently found, and left-sided heart defects are the rule.
Watson syndrome:
Is characterized by short stature, pulmonary valve stenosis, variable intellectual development, and skin pigment changes (e.g., café au lait patches).
Cardiofaciocutaneous (CFC) syndrome:
CFC and NS have the greatest overlap in features. In CFC syndrome, intellectual disability is usually more severe, with a higher likelihood of structural central nervous system anomalies; skin pathology is more florid; gastrointestinal problems are more severe and long lasting; and bleeding diathesis is rare. Facial appearance tends to be coarser, dolichocephaly and absent eyebrows are more frequently seen, and blue eyes are less commonly seen.
Costello syndrome shares features with both NS and CFC.
Noonan syndrome-like disorder with loose anagen hair. Most have the classic loose anagen hair.
Noonan syndrome-like disorder with or without JMML (juvenile myelomonocytic leukemia)
Other:
NS should be distinguished from other syndromes/conditions with developmental delay, short stature, congenital heart defects, and distinctive facies, especially the following:
- Williams syndrome
- Aarskog syndrome
- In utero exposure to alcohol or primidone
- Neurofibromatosis 1(NF1)
NF1 shares some features with NS, including short stature, learning difficulties, and café au lait patches.
Dental manifestations:
Baird and De Jong were the first to document seven cases spanning three generations with anomalous maxillary lateral incisors (Baird and De Jong 1972).
Toureno and Park, reported a case with supernumerary teeth and bilateral enlargement of the mental foramen (Toureno and Park 2011).
Mallineni et al. conducted a systematic review on the dental manifestations seen in association with Noonan syndrome (Mallineni, Yung Yiu et al. 2014). The common oral manifestations included micrognathia, high arch palate, malocclusion, impacted teeth, Early exfoliation of primary canines (Okada et al. 2003) , retroclined mandibular incisors and giant cells in the jaws (Cohen and Gorlin 1991). hypoplastic jaws, retrognathic maxilla and prognathic mandible , labial hypotonia, gingival inflammation, proclined incisors, supernumerary teeth , gingival enlargement, crowding associated with a midline diastema, taurodontism, idiopathic osteosclerosis, hypodontia , deep-bite, asymmetry of tooth morphology of maxillary first molars .
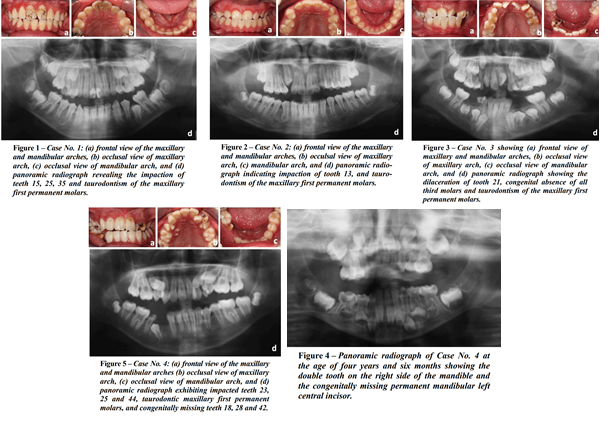
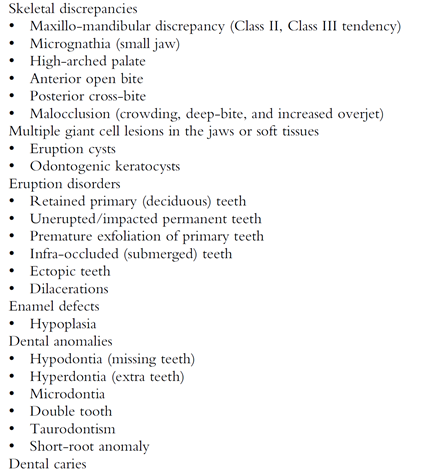

Dental treatment:
The treatment goal is to provide a balanced facial profile and improved function (Anthonappa and King 2019).
- extraction of both retained primary and/or permanent teeth
- surgical removal of supernumerary teeth and/or impacted teeth
- functional appliance therapy
- orthodontic treatment with orthognathic
Bleeding diathesis:
Patients with NS have a history of abnormal bleeding or bruising. Early studies reported that about one third of all individuals with NS have one or more coagulation defects with subsequent studies suggesting a lower rate of coagulopathy (Derbent et al. 2010). The coagulopathy may manifest as severe surgical hemorrhage, clinically mild bruising, or laboratory abnormalities with no clinical consequences. This is important if these patients need surgical treatments or extractions.
Klinefelter Syndrome (KS)
Description:
KS was first described by an endocrinologist ,Harry Klinefelter in 1942 (Klinefelter Jr et al. 1942). KS describes a set of physical, language, and social development symptoms in males who have an extra X chromosome. This can be inherited from either parent (Growth et al. 2013). Its main feature is infertility.
Other names:
- XXY Syndrome
- 47,XXY (most common)
- XXY syndrome or condition
- XXY trisomy
- 47,XXY/46,XY or mosaic syndrome (rare variation)
- Klinefelter-Reifenstein-Albright syndrome
- Poly-X Klinefelter syndrome, including the following rare variations:
- 48,XXYY (or tetrasomy)
- 48,XXXY (or tetrasomy)
- 49,XXXXY (or pentasomy)
Prevalence:
XXY aneuploidy is the most common type with the prevalence of one in 500 males. 48,XXYY and 48,XXXY being present in 1 per 17,000 to 1 per 50,000 male births. The incidence of 49,XXXXY is 1 per 85,000 to 100,000 male births. In addition, 46,XX males also exist and it is caused by translocation of Y material including sex determining region (SRY) to the X chromosome during paternal meiosis (Visootsak and Graham 2006).
Herlihy et al. reported a prevalence of 2.23 per 1000 in an Australian study (Herlihy et al. 2011).
A more recent review has reported the prevalence to be 1:650 newborn males (Kanakis and Nieschlag 2018).
Genetics:
In 1952, KS was characterized by a supernumerary X chromosome in males (Jacobs and Strong 1959). KS occurs when paired X chromosomes fail to separate (nondisjunction in stage I or II of meiosis, during oogenesis or spermatogenesis) (Thomas and Hassold 2003). Both maternal and paternal meiotic nondisjunction can cause KS. Meiosis I error occurs in 75% of maternal nondisjunctions and is associated with increases maternal age. Parental age has also been linked to increase risk of KS but not proved(Lowe et al. 2001).
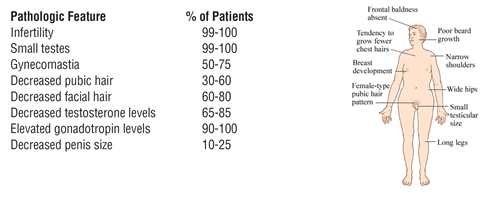
Characteristics:
Not all patients with KS show the same phenotype of the syndrome and there is no one symptom that can define this syndrome.
While Gonadotropin levels are elevated in KS patients, testosterone levels are reduced. Classical characteristics of this syndrome include (Smyth and Bremner 1998):
- Narrow shoulders
- Broad hips
- Absence or sparse facial, axillary, pubic and body hair
- Gynecomastia & Feminine distribution of adipose tissue
- Small testes and penis
- Androgen deficiency
- Reduced intelligence
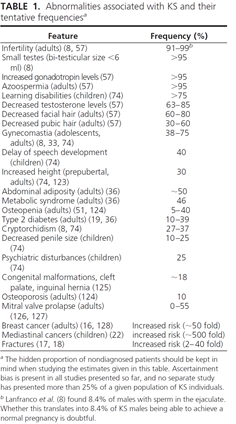
The distribution of clinical and laboratory values in classic KS are shown in the following tabulation (Paulsen et al. 1968):
Abnormalities associated with KS have been summarized in the table blow (Groth et al. 2013):
Frequently associated medical disorders (Sokol 2012):
- Poor muscle tone and strength, as well as impaired gross and fine motor skills, coordination, dexterity, and running ability, can be seen in KS patients.
- Cognitive phenotype is manifested as deficits in the specific domains of language and executive functions. Expressive language is affected more than comprehension or receptive language skills. A study by Skakkebæk et al suggested executive cognitive functions are impacted by their social engagements. Decreased intelligence and lower social skills can be the cause of impaired executive functions (Skakkebaek et al. 2017).
- Schizophrenia, psychosis, and bipolar disorder have been reported in males with Klinefelter syndrome (Boks et al. 2007)
- Tumors/Cancer Mediastinal tumors may occur in young patients (Volkl et al. 2006). Breast cancer and testicular cancer are reported, although a clear relationship between Klinefelter syndrome and testicular cancer has not been documented.
- Vascular disease: Vascular diseases associated with Klinefelter syndrome include hypostatic ulceration, deep vein thrombosis, pulmonary embolism, and ischemic heart disease.
- Endocrine/metabolic and autoimmune diseases Hypogonadism (pathognomonic) and associated osteoporosis occur. Bone density decreases in 25% of males with Klinefelter syndrome, with this most likely being related to decreased bone formation, increased bone resorption, and/or hypogonadism. An increased incidence of diabetes mellitus, obesity, hypothyroidism, Sjögren syndrome, rheumatoid arthritis, and systemic lupus erythematosus have been reported in males with Klinefelter syndrome.
- Dental: Taurodontism (1% in XY males).
Diagnosis:
KS can be diagnosed prenatally from fetal cytogenetic analyses. After birth patients with KS may demonstrate subtle, age related clinical signs. Sometimes their clinical presentation is similar to XY males and diagnosis without karyotyping is difficult. Karyotype analysis is done on peripheral blood lymphocytes.
Other diagnostic tests include:
- XCAT-KS buccal swab test
- fluorescence in-situ hybridization (FISH)
- microarrays
There has been reports about late diagnosis or underdiagnosis of the KS syndrome. This could be due to (Herlihy et al. 2011):
- patients being embarrassed to seek medical attention
- health professionals not being familiar with this syndrome
- medical practitioners not performing routine genital examinations in adult men
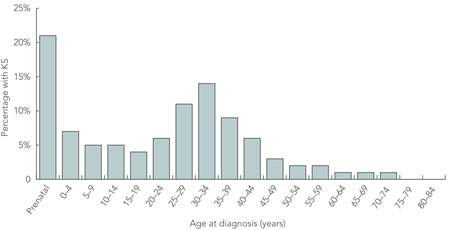
The graph below shows the proportion of males diagnosed with KC in Victoria, Australia, 1991-2006, by age of diagnosis (Herlihy et al. 2011).